Borderline Personality Disorder (BPD) is a complex mental health condition characterized by intense emotional instability, impulsive behaviors, and difficulty in maintaining relationships. Often misunderstood and stigmatized, BPD affects millions of people, causing distress for both the individuals experiencing it and their loved ones. This article aims to demystify BPD by exploring its causes, symptoms, effects, and treatment options, including a closer look at Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
BPD in the USA: An Overview

Individuals with borderline personality disorder (BPD) face a significantly higher risk of suicide, with a rate of 5.9% compared to 1.4% for those diagnosed with other personality disorders. Research indicates that over 75% of people with BPD have attempted suicide, highlighting the serious nature of this mental health condition. Alongside an elevated suicide risk, BPD is associated with a range of medical complications, such as obesity, diabetes, gastrointestinal problems, cardiovascular diseases, hypertension, chronic pain, and sexually transmitted infections. Additionally, the disorder often coexists with other mental health conditions, including mood disorders, eating disorders, post-traumatic stress disorder (PTSD), and substance use disorders. This complex interplay of physical and psychological challenges can reduce life expectancy and makes navigating the healthcare system particularly difficult for individuals with BPD.
In the United States, around 1.4% of adults are diagnosed with BPD, though this number may be underestimated because the disorder’s symptoms often overlap with those of other mental health conditions, complicating diagnosis. Women are disproportionately affected, accounting for about 75% of BPD cases. Despite its prevalence, BPD remains one of the most misunderstood and stigmatized mental disorders, which exacerbates the difficulties faced by those living with the condition.
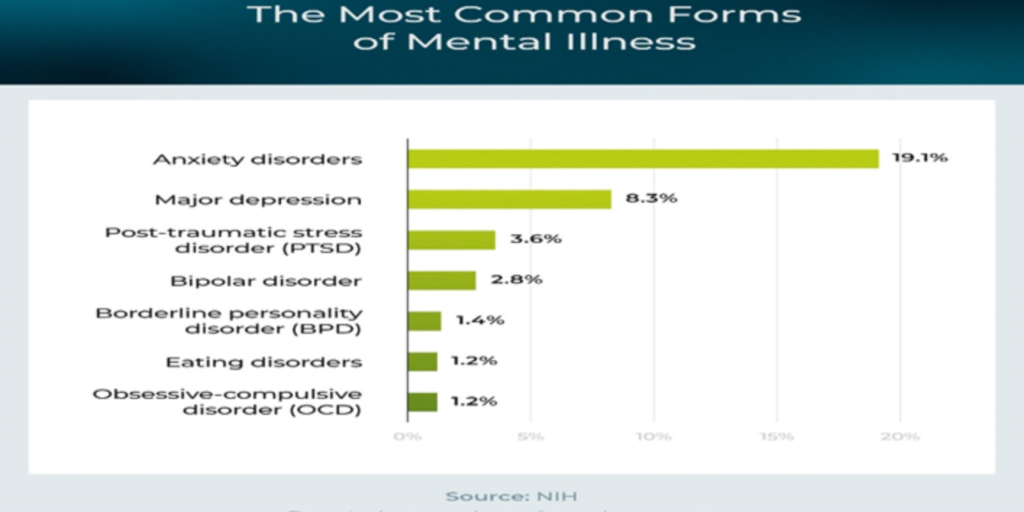
The prevalence of BPD is part of a broader mental health landscape in the U.S., where the National Institute of Mental Health (NIMH) provides data on various disorders. Anxiety disorders top the list, affecting 19.1% of adults, followed by major depressive disorder at 8.3%. PTSD affects 3.6%, while bipolar disorder is reported in 2.8% of the population. BPD, at 1.4%, shares a similar prevalence rate with binge eating disorder and obsessive-compulsive disorder (OCD), each affecting 1.2% of adults. Schizophrenia is less common, with prevalence estimates ranging from 0.25% to 0.64%. These statistics underscore the significant burden that mental health issues place on the adult population, illustrating the need for greater awareness and comprehensive care.
Causes of BPD
The exact cause of BPD is not fully understood, but it is believed to arise from a combination of genetic, environmental, and social factors:
- Genetics: There is evidence suggesting that BPD may run in families, indicating a possible genetic predisposition.
- Childhood trauma: Many individuals with BPD report histories of traumatic experiences, such as abuse, neglect, or significant losses during childhood.
- Brain structure and function: Studies have shown abnormalities in the brain regions responsible for emotional regulation and impulse control in individuals with BPD.
- Environmental factors: Stressful or unstable environments, especially during developmental years, may contribute to the development of BPD.
Effects of BPD
BPD can significantly impact various aspects of a person’s life:
- Interpersonal relationships: Individuals with BPD often struggle with unstable and intense relationships due to fear of abandonment, mood swings, and impulsive actions.
- Self-image and identity: People with BPD may experience an unstable self-image or a lack of sense of self, leading to frequent changes in goals, values, and life ambitions.
- Emotional health: The condition often results in mood instability, with emotions shifting rapidly from intense joy to deep despair.
- Physical health: BPD is associated with self-harming behaviors, such as cutting, and a higher risk of suicidal thoughts and attempts.
Symptoms of BPD
The symptoms of BPD can vary but generally include:
- Intense fear of abandonment, whether real or perceived
- Unstable and chaotic relationships
- Rapid changes in self-identity and self-esteem
- Impulsive and often self-damaging behaviors (e.g., substance abuse, reckless driving)
- Recurrent suicidal behavior, threats, or self-harm
- Emotional instability, with episodes of intense sadness, irritability, or anxiety
- Feelings of emptiness
- Difficulty controlling anger or experiencing intense and inappropriate anger
Treatment for Borderline Personality Disorder
Psychotherapy
Medication (when necessary)
The treatment approach for borderline personality disorder (BPD) generally follows similar guidelines as other personality disorders. It is crucial to identify and address any co-occurring conditions for the treatment to be effective.
Psychotherapy
Psychotherapy serves as the cornerstone for managing BPD. Various therapeutic methods have been proven to help reduce self-harming behaviors, alleviate depression, and improve overall functioning. Key psychotherapeutic approaches include:
- Cognitive-Behavioral Therapy (CBT): Focuses on managing emotional instability and improving social skills.
- Dialectical Behavior Therapy (DBT): Combines individual and group therapy sessions where therapists act as behavior coaches and are available for support around the clock.
- Systems Training for Emotional Predictability and Problem Solving (STEPPS): Involves 20 weeks of weekly group sessions, teaching participants how to handle emotions, challenge negative expectations, and maintain self-care habits. Skills covered include goal setting, avoiding substance abuse, and improving lifestyle habits related to sleep, diet, and exercise. Patients also create a support network of friends, family, and healthcare professionals.
Other therapies address the way individuals with BPD experience emotions and their relationships with others. These include:
- Mentalization-Based Treatment (MBT): Helps individuals understand their own and others’ mental states, fostering emotional regulation and enhancing empathy and compassion.
- Transference-Focused Psychotherapy (TFP): Centers on interactions between the patient and therapist, encouraging patients to reflect on their feelings and reactions during therapy to build a more stable and realistic self-concept.
- Schema-Focused Therapy: Integrates elements of CBT, attachment theory, and other approaches to address long-standing maladaptive patterns (schemas) in thinking, feeling, and behavior. The therapy is divided into three stages: identifying schemas, recognizing them in everyday life, and replacing negative patterns with healthier behaviors.
While many psychotherapeutic treatments for BPD require specialized training, “good psychiatric management” provides a general approach that clinicians can follow. It includes weekly individual therapy sessions, education on the disorder, and treatment expectations, sometimes incorporating medications. This method emphasizes the patient’s response to everyday interpersonal stressors.
Supportive Psychotherapy can also be helpful in establishing a constructive, empathetic relationship with the patient, aimed at fostering healthier defense mechanisms, especially in social relationships.
A Closer Look at CBT and DBT
Cognitive Behavioral Therapy (CBT)

CBT focuses on identifying and changing negative thought patterns and behaviors that contribute to BPD symptoms. It helps individuals recognize how their thoughts influence their emotions and behaviors, offering strategies to break the cycle of negativity. For example, someone with BPD may learn to challenge their fear of abandonment by testing their thoughts against evidence rather than reacting impulsively.
CBT typically involves:
- Cognitive restructuring: Identifying distorted thoughts and replacing them with more balanced thinking.
- Behavioral interventions: Encouraging activities that help improve mood and reduce unhealthy coping mechanisms.
- Skills training: Teaching emotional regulation and problem-solving skills to better manage day-to-day challenges.
Dialectical Behavior Therapy (DBT)
DBT is a form of CBT specifically designed for individuals with BPD. It emphasizes the balance between accepting oneself and making positive changes. DBT has four core components:
- Mindfulness: Focusing on the present moment without judgment to reduce impulsivity and increase awareness.
- Distress tolerance: Learning skills to cope with emotional crises and tolerate distress without resorting to self-harm.
- Emotion regulation: Understanding and managing intense emotions to prevent overwhelming feelings from controlling behavior.
- Interpersonal effectiveness: Building skills to communicate needs assertively and maintain healthier relationships.
DBT’s structured approach has been shown to reduce self-harming behaviors, suicidal ideation, and symptoms of depression in individuals with BPD.
Real-Life Examples of BPD
- Case 1: Sarah struggles with intense fear of abandonment, leading to frequent breakups with her partner due to her unpredictable mood swings. With DBT, she learns distress tolerance techniques that help her manage overwhelming emotions and reduce impulsive reactions.
- Case 2: John has difficulty maintaining stable employment due to his rapidly changing goals and impulsive decisions. Through CBT, he gains insight into his thought patterns, allowing him to challenge his negative self-perceptions and set more realistic career goals.
Medications
Medications are not consistently effective for treating the core symptoms of BPD and are typically reserved for managing specific co-occurring psychiatric conditions (e.g., major depression). When used, options may include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Usually well-tolerated but only moderately effective in alleviating anxiety and depression in BPD patients.
- Mood Stabilizers: May help with mood swings, impulsivity, and symptoms of anxiety or depression.
- Atypical Antipsychotics: Can be used for managing anxiety, mood instability, anger, and cognitive distortions such as paranoid thoughts or black-and-white thinking.
Benzodiazepines and stimulants are generally discouraged due to risks of dependency, overdose, and disinhibition.
Present Psychiatry: Your Partner in Mental Health
At Present Psychiatry, our expert team is dedicated to providing compassionate, evidence-based treatment for individuals dealing with borderline personality disorder. Our services include a variety of psychotherapies, such as DBT and MBT, tailored to meet your unique needs. We are committed to guiding you through the path to mental wellness.
“Therapy is not about fixing someone; it’s about helping them find the stability and understanding they deserve.” — Dr. Rizwan Ali, Present Psychiatry.
Start your journey towards healing today with the support of our experienced team. Let us help you navigate the path to a balanced and fulfilling life.
Reference: National Institute of Mental Health, “Mental Illness,” National Institute of Mental Health, last modified March 2023
WE STRIVE HARD AND PROMISE TO DELIVER
- 5600 NW Central Dr Suite 280, Houston, TX 77092, United States
- +1 832-552-1578
- inquire@presentpsychiatry.com



